FAQ
Visual Field Testing (Perimetry)
- How many degrees does the tablet visual field test cover?
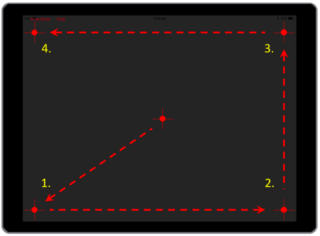
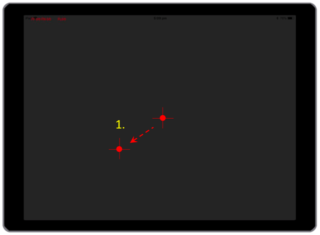
Full threshold visual field testing up to 30 degrees from central fixation point is achieved on standard iPad (9.7 inch) or 10.5-inch iPad pro by patients changing fixation. For the standard iPad (9.7 inch)4 refixations are made to the 4 corners of the iPad to achieve this eccentricity (see left panel below). This is achieved by following the fixation marker (red target) when directed during the test. The iPad pro is larger and only needs 1 refixation, as directed by the voice instruction.
This change in fixation allows visual field testing out to 30 degrees in the horizontal meridian and 24 degrees in the vertical meridian, suitable for visual field assessment.
 |
 |
- What is the threshold provided by MRF Visual field test?
MRF Visual field can return a 30dB threshold across all locations. MRF can achieve this by controlling the size of the dots with respect to the distance from the centre. In contrast, HFA can provide much larger range of brightness for a fixed size. Calibrations show that the brightness of MRF 30 dB corresponds to about 38 dB on a Humphrey perimeter.
- What is the normative database used for MRF apps?
MRF research has measured thresholds in more than 400 cases (124 normal age 19-92; and 280 with eye disease: 92 Glaucoma, age 43-88; 68 AMD, age 62-96; 74 Diabetes, 26-69; 46 Neurological cases age 23-85) and has developed a normative database for the Probability Density Function at each point in the visual field. The fact that our clinical trials show very strong association with Humphrey outcomes indicates that the database is highly accurate.
The normative database comprises people from all ethnicities including about one third as Asians.
- What principle does MRF use for visual field testing?
MRF uses a Bayesian predictor for returning the visual field threshold given a patient’s response matrix to spots of different brightness. It can achieve results equivalent to standard equipment in 1.5 minutes less test time with a similar level of accuracy. This approach is similar to that adopted by Humphrey in their testing technique called SITA but it has been optimised to return fast and reliable outcomes.
- Does the MRF device detect blind spot/scotoma? If yes, how and where is it visible in the results?
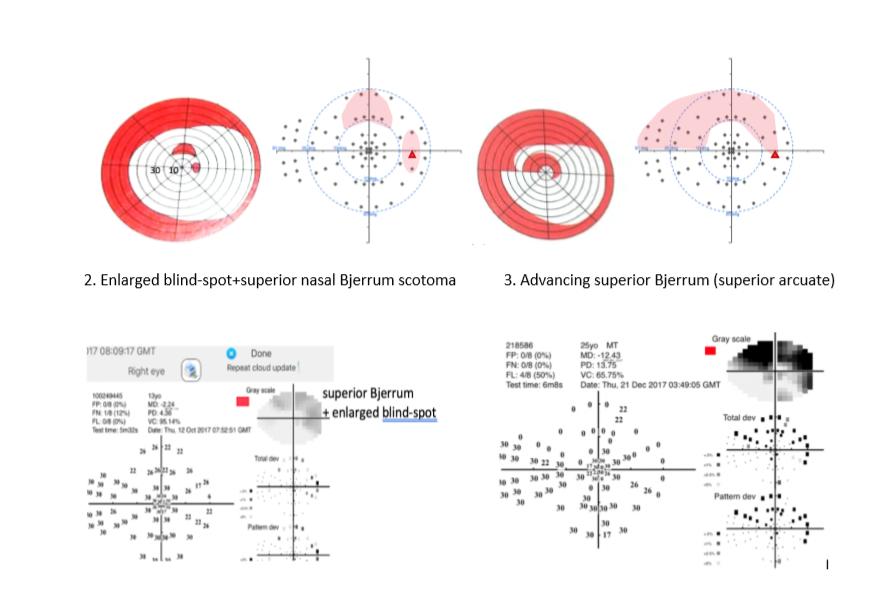
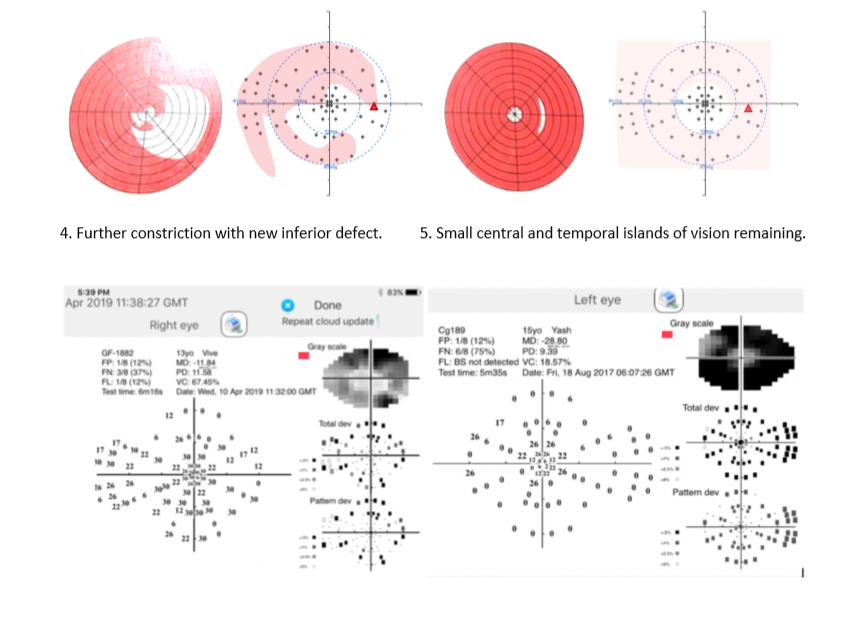
YES, the MRF uses a blind-spot monitor to gauge fixation accuracy. This procedure is common to most perimeters and it starts the test by locating the person’s blind spot. Thereafter it shows spots in the blind spot with the expectation that they should not be seen if fixation is accurate. In our printout the blind spot is shown as a large gap in the graphic. I have shown it as a RED triangle in the below cases to help visualise its location. In some patients the blind spot cannot be detected reliably, and this is recorded on the printout.
- What enhancements does MRF perimeter bring over current generation of automated perimeters?
Current generation of perimeters do not include enhancements learned over the past 30 years. In fact, the grid and test approaches (spot size) are the same as those of the past. In this aspect nothing has changed, and we are still using the dated approaches of Goldmann.
There is now a large body of evidence that shows that the standard (24-2 and 30-2) grids under-sample the macula, the region of highest density of retinal ganglion cells, so in many cases clinicians need to put patients through a second test, the 10-2. What a pain for both the patient and the clinician.
Carl Zeis recently addressed macula under-sampling by developing 24-2C grid. The new grid has an extra 10 points within the central 10 degrees for a total of 22 macula test points. However, this compares poorly to the 68 points of a 10-2 grid over the same area.
24-2C has been optimised for glaucoma but will they cope with the more common causes of central vision loss such as AMD or macular oedema?
Since vision loss varies with disease, MRF is optimised to include four grid patterns specific to glaucoma, maculopathy/AMD, diabetes and neural diseases.
The novel implementations in these designs are a spot size that increases with eccentricity to reduce threshold variability: an expanding test grid to define edges of vision loss and a Bayes threshold predictor with neighbourhood logic to return fast, reliable thresholds (2-3 minutes).
Moreover, MRF includes three forms of acuity testing that identify refractive/optical changes, retinal or brain losses.
- Does the device detect fixation loss? If yes, how does it do it (via camera?)?
At present the MRF uses a blind-spot monitor to detect fixation loss (see above point 5).
For those who are interested, an independent clinical trial performed in Sydney by Dr Stuart Grahams group reached the below conclusion
Please refer to this report “Schulz et al. Performance of iPad-based threshold perimetry in glaucoma and controls. Clinical and Experimental Ophthalmology 2018; 46: 346– 355 doi: 10.1111/ceo.13082”
- Do we have visual field clinical trials or test data for Asian/Indian patients or cohorts?
Yes, the MRF has been used extensively by Dr Viney Gupta and his team (Dept of Ophthalmology (R.P.C) AIIMS, New Delhi). His findings on 21 glaucoma adults have been published as part of a large clinical trial including 39 cases tested in Cambridge UK and his recent work on 43 eyes of 26 children with congenital glaucoma are presently being analysed. We will forward copies of publications on request.
Acuity Testing
- What is the purpose of Low Contrast Low luminance acuity test?
Low Contrast Low Luminance (LLLC) acuity test is great for detecting disorder of retinal pathology. Macular function can be assessed using LLLC in adults with Type 2 Diabetes Mellitus.
As per research, Smith–Kettlewell Institute Low Luminance (SKILL) Card demonstrates vision function changes in diabetes even in the absence of clinically evident retinopathy. Diabetic retinopathy leads to a further increase in SKILL score, while high contrast VA remains unchanged and standard contrast sensitivity also shows marginal effects.
The research is titled “Assessment of Macular Function Using the SKILL Card in
Adults with Type 2 Diabetes Mellitus” and is available on request.
- How are Low Luminance Low Contrast acuity test results interpreted?
Low Luminance Low Contrast (LLLC – labelled ‘Low contrast Snellen’) is expected to be 6/12 or better for healthy macula and retinal function. The Smith–Kettlewell Institute Low Luminance (SKILL) Card has been used in patients with type 2 diabetes mellitus (T2DM) and been found to have a high sensitivity to abnormal retinal function caused by diabetes. The LLLC charts can be used to evaluate the impact of reduced contrast and reduced luminance on visual acuity.
LLLC vision testing has been found to predict subsequent acuity loss in an aged population as per research. Tests of low contrast spatial vision are strong predictors of early retinal dysfunction. These findings have implications for clinical trials, clinical management, and acceptance of these measures into clinical practice.
The research is titled “Low contrast vision function predicts subsequent acuity loss
in an aged population: the SKI study” and the research paper is available on request.
- How can MRF apps be used for detecting eye issues related to diabetes in advance?
Visual Field Testing
- 8% of participants with Diabetes return an abnormal Visual Field Test although their retina is normal
The incidence of visual field loss increases to 65% with severe diabetic retinopathy - Vision loss can predict the future development of retinopathy by up to 18 months. These people need to be monitored closely to ensure prompt medical intervention (Bearse et al. Prog Retin Eye Res 2006; 259(5):425-48)
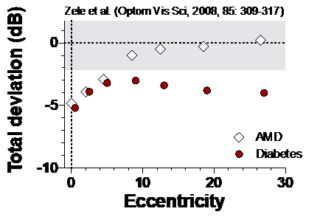
Patients with early diabetes show a loss of
sensitivity across the visual field.
Low Contrast Acuity Tests
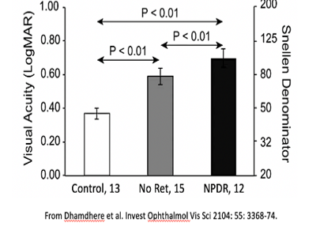
- 81% of people who were Diabetic for 9.5 years, but who did not have Retinopathy, were found to be abnormal on this test (Dhamdhere et al. Invest Ophthalmol Vis Sci 2104: 55: 3368-74)
- The test will also detect developing cataract – a common complication of diabetes.
The specific tests for Diabetes related eye issues are:
-
- Visual Field Test
- Full Visual Field Test (3.5 minutes)
- Macula 10-2 test
- Visual Field Test
Acuity Tests
-
-
- Low Luminance Low Contrast (for Diabetes)
- High Contrast Acuity
-
